
The Problem With “Over-Exfoliation Culture”
The skincare industry’s obsession with “instant glow” has normalized chronic exfoliation — a silent epidemic that damages the skin barrier, disrupts its microbiome, and accelerates inflammation-driven aging. This article breaks down what really happens beneath the surface when you overuse acids, the clinical markers of barrier burnout, and evidence-backed steps to restore balance.
Note: The content provided by Cordeo is for informational and educational purposes only and does not constitute medical advice, diagnosis or treatment. Always consult a qualified health provider for advice regarding your specific medical condition. [See Full Disclaimer]
The Rise of Over-Exfoliation Culture
There’s no denying that exfoliation has revolutionized skincare. Alpha and beta hydroxy acids (AHAs and BHAs) — like glycolic, lactic, and salicylic acid — are proven to improve texture, even tone, and enhance cell turnover. But what began as a dermatologist-supervised treatment quickly turned into a social media challenge: “10-minute miracle,” “peel challenge,” “daily resurfacer.”
This “peel culture” pushes consumers to exfoliate daily or even layer multiple acids together — far beyond what the skin barrier can physiologically handle.
The stratum corneum, the outermost layer of the epidermis, naturally desquamates every 28 days (slower in dry, mature, or sensitive skin). Exfoliation helps accelerate this, but excessive chemical or physical exfoliation removes not only dead corneocytes but also vital intercellular lipids, weakening the barrier [1].
Barrier Burnout: The Modern Epidermal Fatigue
Once the skin barrier is weakened, the innate immune system becomes hyperactive. This leads to a condition dermatologists refer to as barrier fatigue — a chronic, subclinical inflammation marked by persistent redness, sensitivity, and dullness.
Over time, this low-grade inflammation contributes to inflammaging — premature aging driven by inflammatory cytokines that degrade collagen and elastin [6].
In short: over-exfoliation not only makes your skin temporarily sensitive — it makes it age faster.
What Happens Beneath the Surface When You Over-Exfoliate
Think of your skin barrier as a brick wall — corneocytes are the “bricks” and lipids (ceramides, cholesterol, fatty acids) are the “mortar.” Acids, when used in high concentrations or too frequently, dissolve that mortar.
When the lipid matrix is disrupted, the barrier loses its ability to regulate water and defend against irritants. Clinically, this manifests as increased transepidermal water loss (TEWL), microfissuring, and pro-inflammatory signaling within keratinocytes [2][3].
Biopsies from over-exfoliated skin show:
Depleted intercellular lipids (especially ceramides 1, 3, and 6-II)
Increased IL-1α, TNF-α, and IL-8 levels — markers of inflammation and irritation [4]
Disruption of tight junction proteins like claudin-1 and occludin, compromising barrier cohesion [5]
Translation: your “tingling” sensation isn’t proof of effectiveness — it’s a micro-inflammatory cascade your skin is begging you to stop.


The Hidden Impact on the Skin Microbiome
A balanced microbiome acts as the first line of defense against pathogens. Acid misuse alters the skin’s pH and lipid content, disrupting commensal bacteria like Staphylococcus epidermidis and Cutibacterium acnes that maintain immune balance [7].
When this ecosystem is disturbed, opportunistic microbes thrive, worsening acne, rosacea, and dermatitis. Restoring this balance requires not just hydration but microbiome-friendly lipids and prebiotic repair ingredients.
Clinical Signs of Over-Exfoliation
If you’re wondering whether your skin barrier is compromised, here’s what to look for:
Persistent redness, burning, or stinging
Tightness or shiny, “plastic-like” texture
Sudden breakouts or papular eruptions
Flaking, itching, or sensitivity to water
Uneven tone or hyperpigmentation (especially in medium to dark skin)
Poor tolerance to active ingredients or sunscreen
When these symptoms appear, immediate cessation of exfoliants is non-negotiable.
How to Clinically Restore a Damaged Barrier
Barrier repair isn’t just about “moisturizing more.” It’s about biochemical replacement and physiologic healing.
1. Discontinue Actives
Stop AHAs, BHAs, PHAs, and retinoids for 10–21 days. Allow your keratinocyte renewal cycle to stabilize naturally.
2. Replace Lipids Intelligently
Replenish the lipid matrix using moisturizers that mimic the natural 3:1:1 ratio of ceramides:cholesterol:fatty acids — a ratio clinically shown to accelerate barrier recovery [8].
Example actives: ceramide NP, phytosphingosine, cholesterol, linoleic acid.
3. Hydrate Without Overloading
Prefer glycerin, panthenol, and urea (≤5%) as humectants. Avoid heavy hyaluronic acid layering during active inflammation — it can worsen TEWL in dry climates [9].
4. Calm the Inflammation
Use anti-inflammatory molecules such as ectoin, Centella asiatica, and allantoin — all of which stabilize cell membranes, reduce oxidative stress, and restore hydration [10][11].
5. Protect During Recovery
Daily use of broad-spectrum SPF and non-foaming, pH-balanced cleansers (4.5–5.5) is essential. Avoid physical scrubs and fragranced products until sensitivity subsides.
Barrier repair typically takes 2–4 weeks, depending on the depth of damage.
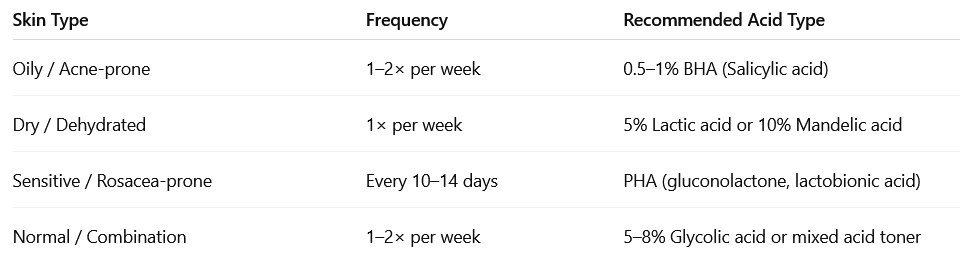
When and How to Reintroduce Exfoliation
Once your skin has normalized — no redness, no stinging, no tightness — you can safely reintroduce exfoliants.
Here’s a clinical approach:

Professional Perspective
From a professional standpoint, the purpose of exfoliation is controlled regeneration, not chemical aggression. Epidermal health depends on maintaining a stable lipid barrier and balanced desquamation rate.
Healthy skin glows because of structural integrity, not because it’s been stripped raw. The ultimate goal isn’t faster exfoliation — it’s smarter rejuvenation.
REFERENCES
Rawlings AV, Harding CR. Moisturization and skin barrier function. Dermatologic Therapy. 2004;17(1):43–48.
Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Experimental Dermatology. 2008;17(12):1063–1072.
Elias PM, Williams ML. Re-appraisal of current theories for the development and loss of the epidermal barrier. Experimental Dermatology. 2013;22(7):499–502.
Wilhelm KP et al. Effects of glycolic acid on human skin barrier function. Br J Dermatol. 1993;129(5):537–544.
Kirschner N et al. Tight junctions and the epidermal barrier. J Clin Invest. 2013;123(3):956–965.
Krutmann J et al. Inflammaging and photoaging: Evidence and molecular mechanisms. J Invest Dermatol. 2017;137(5):1027–1031.
Sanford JA, Gallo RL. Functions of the skin microbiota in health and disease. Semin Immunol. 2013;25(5):370–377.
Man M-Q et al. Re-establishment of stratum corneum lipids by topical physiological lipid mixtures. J Invest Dermatol. 1996;106(5):1096–1101.
Lodén M. The clinical benefit of moisturizers. J Eur Acad Dermatol Venereol. 2005;19(6):672–688.
Peirano RI et al. Ectoine in dermatology: Stabilization of biomolecules and barrier protection. J Clin Aesthet Dermatol. 2011;4(9):45–53.
Kim JY, Kim MH, Kim YS et al. The effects of Centella asiatica extract on barrier function and inflammation. Int J Mol Sci. 2018;19(10):E3048.
CORDEO
FOR CONATCT:
© 2025. All rights reserved.
Rooted in science. Built with integrity. Designed to empower.
HOME
ABOUT
THE HEALTH EDIT
SKIN BY CORDEO
NOURISH BY CORDEO
MED JOURNAL
CORDEO SHOP
THE HEALTH ORBIT
CORDEO LETTER
THE DIGITAL HUB
CORDEO CONSULTS
CONTACT US
COMING SOON
Cordeo is a digital wellness platform that offers medically-informed content and curated tools for holistic health. The content on this site is for informational and educational purposes only and does not constitute professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalized medical guidance.
By using this website, you acknowledge and agree to our Disclaimer, Privacy Policy, Terms & Conditions, Cookie Policy, Editorial Policy, and User Conduct Agreement.
Affiliate & Sponsorship Notice: Some content may include affiliate links, and we may earn a commission on qualifying purchases — at no extra cost to you. We do not process refunds for affiliate partner products or services.
For comprehensive legal and compliance information, please visit our legal and policy center.
This site is governed by the applicable laws of India.
© 2025 Cordeo. All rights reserved. | This site is for informational and educational purposes only and does not constitute professional medical advice.
📢 Cookie & Data Use Notice
We use cookies and similar technologies to enhance your browsing experience, analyze site traffic, and personalize content. By continuing to use this site, you agree to our use of cookies in accordance with our Cookie Policy.
You can manage your preferences or opt-out of non-essential cookies anytime.